У складу са својом мисијом, Уредништво МедТвоиЛокони улаже све напоре да обезбеди поуздане медицинске садржаје подржане најновијим научним сазнањима. Додатна ознака „Проверен садржај“ означава да је чланак прегледао или директно написао лекар. Ова верификација у два корака: медицински новинар и лекар нам омогућава да пружимо најквалитетнији садржај у складу са тренутним медицинским сазнањима.
Наше залагање у овој области оценило је, између осталих, и Удружење новинара за здравље, које је Редакцији МедТвоиЛоконија доделило почасну титулу Велики просветитељ.
40 percent of Europeans suffer from mental disorders. Fears dominate. The drug was supposed to be benzodiazepines. They quickly suppress anxiety and put you to sleep. Doctors wrote them out to desperate patients without hesitation. It turned out that when used inappropriately, they are addictive, increase anxiety, and cause memory gaps. Should you be afraid of benzodiazepines and how to fight anxiety? Zuzanna Opolska, a MedTvoiLokony journalist, asks an outstanding psychiatrist – Sławomir Murawiec, MD, PhD.
- Almost 40% of Europeans suffer from mental disorders. They even outperform heart disease and cancer in statistics. The most common are anxiety disorders
- Desperate patients ask doctors for pills that will quickly reduce anxiety. These prescribe benzodiazepines. It is a group of drugs with rapid anxiolytic, sedative, hypnotic and anticonvulsant effects
- One million Britons are addicted to these drugs, six million Germans take tranquillizers every day. In Poland, the scale of the phenomenon may be similar
Zuzanna Opolska, MedTvoiLokony: Doctor, it is said that benzodiazepines are easy to start taking, but very difficult to stop. Why?
Sławomir Murawiec, MD, PhD: This is a paradox in psychiatry. When we ask patients what they fear about psychiatric drugs, they often say “personality changes” and “addictions.” At the same time, the most popular group of drugs are benzodiazepines. And that’s the only group that’s addictive.
Are they all equally dangerous?
Not. Depending on the half-life, we can distinguish short, medium and long-acting benzodiazepines. The former are especially dangerous.
Зашто?
They have a quick and clear calming effect that wears off after a few hours. Therefore, there is a temptation to reach for another pill and repeat the obtained effect. Every time we feel anxious, and even forever. Our well-being becomes dependent on taking medications. It’s risky.
Because the farther into the forest, the worse – with time the current dose is not enough for us?
Yes – tolerance to the drug increases. Once the patient has entered addiction mode, we have a vicious cycle. Because over time, he needs doses that are absurdly high, and yet still not getting the desired effect. It is worth emphasizing, however, that benzodiazepines are not incarnate. It’s the same with alcohol – all drinkers, but not all alcoholics. Benzodiazepines pose a risk of addiction, but it’s not that anyone who looks at the pill will become addicted.
These drugs were already used in the 60s, even overused, because only 30 years later guidelines for their safe use were published. Are doctors still recklessly prescribing them today?
Fortunately, this is changing. When I started working, many patients were on off-label benzodiazepines. From general practitioners – family doctors today. I think there was helplessness behind this mechanism. Imagine a patient who has life troubles, is awake, nervous, angry. It hurts here, it leaks over there. She goes to a GP who does all possible examinations, prescribes medications for the stomach, heart and nothing. He still doesn’t know what’s wrong with the sick person. Eventually, the doctor discovers that if he gives a benzodiazepine, the patient gets better. He stops coming and reporting so many ailments. Fortunately, today the awareness of depression is much greater than it used to be, and family doctors are more likely to use antidepressants from the group of selective serotonin reuptake inhibitors (SSRIs) because they know that it is a better method than benzodiazepines.
On the other hand, not so long ago the words “I am depressed” hardly ever passed through the mouth.
That’s true. Depression consists of several groups of symptoms: sadness, anhedonia, which patients describe as: “I am happy, I am not interested in anything”, decreased life activity (driving force), sleep disturbances and anxiety. While benzodiazepines can work on the last element, they do not cure depression. It’s like fighting a fever instead of treating a bacterial infection with an antibiotic. It is not a causal treatment that can help. As a result, we have less anxiety, but we are still sad and still not motivated to act.
Who is especially at risk of benzodiazepine addiction? Is it true that you are addicted to alcohol?
Not only. Clinically, we put it very broadly: people prone to addiction.
Women are more vulnerable than men?
We have different patient groups. Young people experiment with drugs to alter their state of consciousness, and they are often better than the psychiatrists who seek prescriptions know how it works.
Men go to drink more often, and women try to alleviate the problem by “numbing themselves” and inhibiting emotions. Especially middle-aged women who find themselves in a difficult life situation, try to ease the pain of life with pills. Therefore, they more willingly reach for benzodiazepines, which in this case are not a cure for the disorder, but become a way of coping with a difficult life situation.
Some people do not have the dilemma of benzodiazepines or alcohol. They connect them. A tablet plus a glass or a bottle of wine – what’s the risk?
It’s highly threatening. Absolutely not recommended. And when you stop taking medication, the patient is left with several problems: resulting from a difficult life situation, caused by the lack of medicine and alcohol addiction.
The use of benzodiazepines in seniors is controversial. Research confirms that after such drugs, they have an increased risk of falls, and therefore hip fractures.
As with any drug therapy, benzodiazepine treatment has side effects. It is mainly increased sleepiness, impaired concentration, weakness, memory disorders and impaired coordination. If a 20-year-old falls, he will have a few bruises at most, in the case of an 80-year-old we are talking about a life-threatening situation. Therefore, the use of benzodiazepines should be restricted to the point of essential. In addition, the doctor must very strongly warn the patient that such symptoms may appear.
It is said that taking these drugs increases the risk of memory impairment and dementia.
Memory disorders or cognitive decline often occur in people who use benzodiazepines for months or years. Additionally, these patients are mostly apathetic – they have no motivation to act, they are not interested in the world around them.
So when is the use of drugs from this group justified?
If used skillfully, benzodiazepines have many applications because they have a broad spectrum of activity. In neurology, they are used to treat seizures or reduce muscle tension, in premedication anesthesiology, and in psychiatry, they are mainly used in sleep disorders and anxiety disorders.
We have a lot of fears today …
Indeed, there are many more drugs that have an anxiolytic effect. At present, antidepressants or pregabalin are used more often than benzodiazepines. It is a derivative of gamma-aminobutyric acid (GABA).
Patients do not always distinguish between anti-anxiety drugs and antidepressants, which also help with anxiety, but are nevertheless a separate class of drugs.
So shouldn’t benzodiazepines be used to treat depression?
They should definitely not be used as the sole drug, but it is not, again, that they absolutely must not be used. Theoretically, antidepressants take two weeks to work as ‘leafleters’. And if the patient has severe anxiety, apart from the antidepressant, we give him the benzodiazepine at the same time, so that he can live to the two weeks. Then we withdraw it, and the patient stays on the antidepressant.
What about benzodiazepines? When are they still necessary?
They work with anxiety and a particular kind of anxiety – the one that paralyzes, is here and now. It makes us almost stop thinking, we lose control over our emotions and behavior, we feel that we are going crazy.
In anxiety disorders, panic attacks are a good example of their use. The basic treatment in this situation is the administration of drugs from the antidepressant group, they should be taken on a permanent basis. Which does not mean that the patient cannot carry a benzodiazepine – taken on an emergency basis for an anxiety attack, and not every day as part of life problem solving.
Only occasionally, temporarily, because regular use is a certain addiction?
Benzodiazepine drugs can be used on a regular basis. Only short-term – from four to six weeks. Or temporarily with breaks lasting several days. The latter seems to be safer in terms of long-term effects.
And you have to start with the minimum doses?
It depends, there is a relationship between the dose and the treatment effect. It is the strength of anxiety that determines the size of the dose. If someone is very upset, the smallest dose will not help him.
The main problem with benzodiazepines is that they are used off-label. Not so much for solving as for suppressing problems. The pill becomes a reliever of fears, anxieties, awareness of the situation in which we find ourselves – it suppresses the so-called the pain of life.
Benzodiazepine can not be quit overnight?
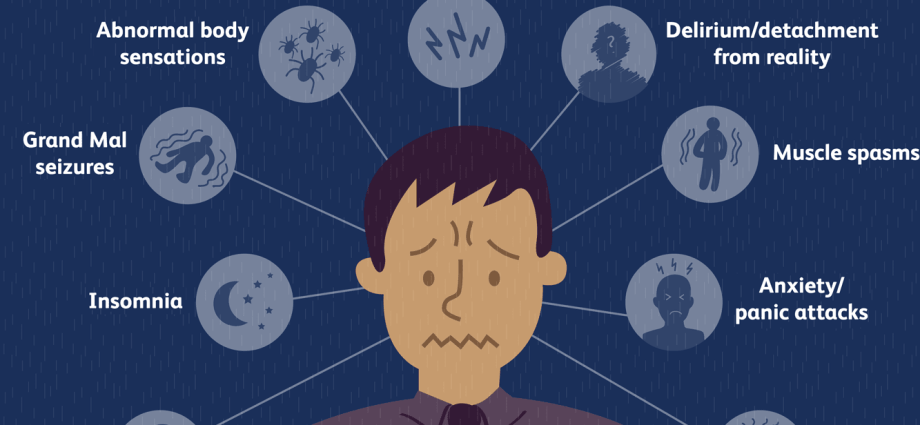
No, unless it is the lowest dose and only taken briefly. On the other hand, if we take benzodiazepine drugs for longer, in a medium or higher dose, then discontinuing them overnight may result in a recurrence of severe anxiety symptoms. And even psychosis, delusions, and seizures.
Sounds a bit like an abstinence syndrome.
Not a little bit, but fully and strong. Safe withdrawal of benzodiazepines is no faster than 1/4 of the dose in a week. These are official medical recommendations, but I would suggest even slower withdrawal.
Sławomir Murawiec, MD, PhD, psychiatrist, psychodynamic psychotherapist. Editor-in-chief of “Psychiatria”, president of the Scientific Society for Psychodynamic Psychotherapy. For many years he was associated with the Institute of Psychiatry and Neurology in Warsaw. Founding member of the International Neuropsychoanalytical Society. Laureate of the Professor Stefan Leder, a distinction awarded by the Polish Psychiatric Association for merits in the field of psychotherapy.